Australian researchers are about to launch a human trial to treat spinal cord injury by transplanting cells from the noses of paralysed patients into the damaged area.
Griffith University scientists have developed tiny biological bridges, each made up of millions of nasal cells, which they hope will encourage nerve cells to regenerate and grow over a patient’s spinal cord injury.
The big hope is that the treatment will result in at least some repair of the spinal cord.
Researcher James St John said even small improvements in function, such as allowing movement in paralysed fingers or restoring bladder and bowel sensation, may boost a person’s quality of life.
The therapy is being developed to potentially help patients such as teenager Joe Pouniu.
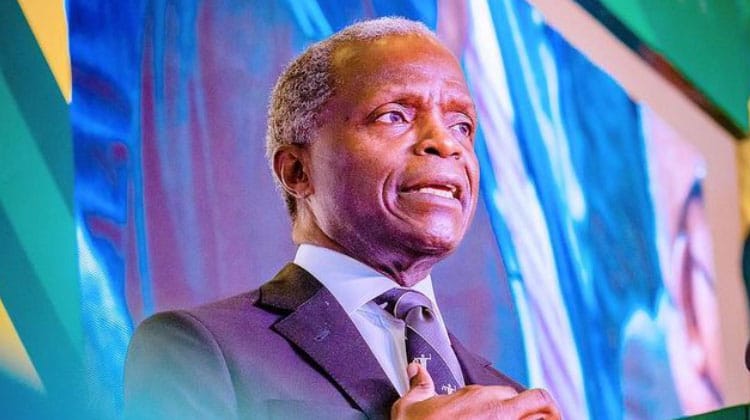
Eighteen-year-old Joe was a promising rugby league player, signed with the Gold Coast Titans, before he ran into a goal post and severed his spinal cord early last year.
Joe lives with quadriplegia but is grateful to have use of his hands.
He’s yet to sign up for the $14 million trial but said even some increases in movement could make “a major difference in our lives”.
“Obviously, people less fortunate don’t have as much function as I do,” he said.
Biological bridges
Professor St John said scans would be used to build a 3D replica of a patient’s spinal column and injured spinal cord, allowing surgeons to prepare for the transplant surgery.
A small biopsy is taken from the inside of a patient’s nose to source cells for the transplant.
Specialised cells, known as olfactory ensheathing cells, are then separated and expanded in the laboratory over several weeks. They can be frozen until the patient is ready for the transplant.
Cell bridges can be prepared for the transplant with a few days’ notice.
Secrecy surrounds the science behind the unique biological bridges, the result of decades of painstaking research at Griffith University.
“The nerve bridges have nothing else in them apart from cells,” Professor St John said.
The scientists are yet to publish their work. Their preference is to wait until a patent can be obtained at an optimal stage in the research, given the need for a huge amount of investor dollars to take the therapy to market, if human trials prove successful. That’s likely to take years.
Professor St John said a neurosurgeon would transplant the cell bridges, each about 2 centimetres long and a couple of millimetres wide, into a patient’s damaged spinal cord and anchor them with surgical glue.
Each cell bridge contains between 5 to 10 million cells, and more than one bridge will be transplanted into each patient’s injured spinal cord.
About 30 patients with spinal cord injury will be recruited for the four-year “world-first” trial — 20 will receive the transplanted cell bridges, along with intensive rehabilitation, while the remaining 10 will just receive rehabilitation.
“Fingers crossed it’s going to work,” said Professor St John, who is the director of Griffith University’s Clem Jones Centre for Neurobiology and Stem Cell Research.
“We’re aiming low and hoping for high. Our primary measure is to look for changes that might be occurring within the spinal cord.
“We can detect those through medical imaging and electrophysiology to show that something has changed.
The work builds on the research of 2017 Australian of the Year, Professor Alan Mackay-Sim, who died last year.
In 2002, Professor Mackay-Sim transplanted olfactory ensheathing cells into the spinal cords of three patients with spinal cord injuries, proving the process was safe.
His published study came off the back of overseas research showing olfactory ensheathing cells, which form part of the sense of smell, allow nerve fibres to be continually renewed, triggering hope they may be useful in spinal cord regeneration.
‘Good recovery’ in trials
A lack of funding prevented Professor Mackay-Sim from furthering the work, but it was resurrected at Griffith University in 2016 under Professor St John.
His team has created nerve bridges from olfactory ensheathing cells, overcoming previous limitations involved in the transplantation of cells directly into the spinal cord.
Professor St John said the cell bridges had proved successful in treating spinal cord injuries in animals, with “good recovery” achieved.
He expects the Griffith University-developed cell bridges to be transplanted into a human spinal cord for the first time next year at a south-east Queensland hospital.
The first patients will have complete spinal cord injuries and be at least 12 months post-injury.
The first part of the trial, which has been approved by a human research ethics committee, will test the cell bridges’ safety, but the scientists’ hope to also assess the therapy’s effectiveness as the study continues.
Eventually, patients with partial spinal cord injuries will be recruited for the study.
Since 2016, about $40 million has been spent on the research to get it to this point, including $14 million for the trial, with significant funding from the Clem Jones Foundation, the Motor Accident Insurance Commission and the Perry Cross Spinal Research Foundation.
Small improvements mean big changes
Joe Pouniu, who has recently taken up wheelchair rugby, is one of about 20,000 Australians living with a spinal cord injury.
He spent 11 months in hospital after his accident, which happened during an under 17 pre-season rugby league trial match between the Future Titans and the Broncos.
Known as “Big Joe”, the 2-metre tall front rower was allowed home in time for his school formal.
While the ultimate goal of a spinal cord injury therapy is to allow a patient to walk again, for Joe and others like him, even small improvements can be important.
“Just to become as independent as I can, obviously do daily life, and be able to get out in the world, just be more free.”
Secrecy around cell bridges
The ABC approached independent experts to comment on next year’s human trial, but they all declined given the lack of published data on the Griffith University cell bridges.
Professor St John defended the team’s strategy as the best chance of ensuring the therapy will be commercialised, if successful.
“I’m sure that we’re going to get criticisms from the worldwide community. There’s no publications around this but that’s just the way life is,” he said.
The potential transformative power of the biological bridges has been recognised by two national research awards — the National Health and Medical Research Council’s Marshall and Warren Innovation Award in 2020 to Professor St John, and the Research Australia Discovery Award in 2020-21 to Dr Mo Chen, who invented the technology to produce them.
Professor St John said the human trial would be open to participants in south-east Queensland, northern NSW, Sydney and Melbourne.
He said some people with spinal cord injuries had relocated to be eligible for possible selection in the trial, some from as far away as the United States.
“I’m not encouraging it. But that’s what some people are doing,” he said, adding that selection for the human study would be done independently of the research team.